Dr. Thomas Mantse is an internationally recognized Canadian physician with more than 33 years of experience in hair transplantation.
There will be no pain after treatment and recovery is very fast. Our motto is "Go back to work the next day!"
Dr. Thomas Mantse
Hair transplantation specialist
Workplaces:
- 2001-2007 "Atlantik" International Hair Transplant Clinic, Budapest - Founding member and primary physician
- 2007- "Prohair" International Hair Transplant Clinic, Budapest, Venezuela - Founding member and primary physician
FUE HAIR TRANSPLANTATION
FUE
What is Follicular Unit Extraction (FUE)
Follicular Unit Extraction (FUE) is a method of obtaining donor hair for Follicular Unit Transplantation (FUT), where individual follicular units are harvested directly from the donor area, without the need for a linear incision. With the FUE technique, a 0.8 mm to 1.0 mm manual punch is used to make a small circular incision in the skin around the upper part of the follicular unit, which is then extracted directly from the scalp. Follicular Unit Transplantation (FUT) and Follicular Unit Extraction (FUE) are sometimes mistakenly viewed as being two totally different hair transplant procedures. FUE, in fact, is a sub-type FUT where the follicular units are extracted directly from the scalp, rather than being microscopically dissected from a strip that has already been removed. To say it another way, in Follicular Unit Transplantation, individual follicular units can be obtained in one of two ways; either through single strip harvesting and stereomicroscopic dissection, or through FUE. Therefore, when comparisons are made between FUT and FUE, what is really being compared is the way the follicular units are obtained (i.e. strip harvesting and dissection vs. direct extraction). The process in the recipient area is the same. The main advantage of FUE is that it does not cause a linear scar. Therefore it is useful in patients who for one reason or another may in the future want to have their donor area very short.
How do we perform FUE hair transplantation?
The hair is shaved (2mm) in the donor area and if the doctor can see the patient's skin. The FUE is removed with a small medical instrument which is a round punch (0.8 mm - 1.0 mm) via a complex process. After the anesthesia, an acute puncture is applied to the skin tissue surrounding the follicular units. It is not always possible to hit the direction of the hair under the skin, so the hair that is cut remains in the donor area and will grow after a few weeks. If the punch is successful, the graft is pulled up with tweezers and a small hole remains which heals after a few days without any visible scaring. In the case of the automated FUE technique, the small holes will leave white dots that is scarring and will remain for life. If the surgeon works manually, as in the PROHAIR CLINIC it will look nothing after a week.
NLHT
NHLT
The FUE brought us to the NO LOOK HAIR TRANSPLANT (NLHT). PROHAIR Transplant Clinic is the only clinic in the world who can perform this technique because we at PROHAIR Transplant Clinic developed it. There are many cases where the normal FUE cannot be used. For example, when there are women patients. Before the NLHT, the only way to treat women was by FUT strip, which means scarring. PROHAIR Transplant Clinic has been performing FUE since 2008 and it has real good uses, but for one and a half years PROHAIR Transplant Clinic could not use FUE on female patients or male patients who did not want to shave their donor areas for many reasons, for instance, there is or are scars noticeable from previous hair transplants or do not want to take time off from work but want to go back to work the very next day. PROHAIR Transplant Clinic performs what is called ”The No Look Hair Transplant” (NLHT). It is called NLHT because there is no need to shave the donor area because only those follicular units (FU) that are needed for transplantation, are cut to 2mm. This way the remaining hairs in the donor area can hide and conceal the areas where they are taken out from. This procedure is ideal for both female and male patients. Please keep in mind that max, 2000 FUE can be transplanted or 1000 FU/day can be used at one time because if more are used then there will not be enough hairs to camouflage.
Consultation
Consultation
WHAT CAN I COUNT ON IN THE FIRST CONSULTATION AT THE PROHAIR CLINIC?
Dr. Thomas Mantse examines the patient's head thoroughly, composes a detailed pathology and determines if the patient is suitable for hair transplantation. If she/he is not suitable, he explains in detail the cause and proposes a possibility of medical therapy. He examines the head and hair. He examines the density of the hair with a special measurement, which determines the density and precisely how many hairs contain the follicular units and what type of alopecia it is. With the instrument, he compares healthy and unhealthy hair, then determines the extent of miniaturization and the diameter of the hairs.
FOR MEN
FOR MEN
MALE PATTERN BALDNESS
Androgenetic alopecia or commonly male pattern hair loss (MPHL) accounts for more than 95% of hair loss in men. By the age of thirty-five, 35% of all Hungarian men will experience some degree of appreciable hair loss and by the age of 50 approximately 50% of men have significantly thinning hair. Approximately twenty five percent of men who suffer with male pattern hair loss begin the painful process before they reach the age of twenty-one. Contrary to societal belief most men who suffer from male pattern hair loss are extremely unhappy with their situation and would do anything to change it. Hair loss affects every aspect of the hair loss sufferer’s life. It affects interpersonal relationships as well as the professional lives of those suffering. It is not uncommon for men to change their career paths because of their hair loss.
CAUSES of HAIR LOSS
Androgenic alopecia or male pattern hair loss (MPHL) is responsible for the vast majority of hair loss in men. While there are many possible reasons people lose hair including serious disease, reaction to certain medications and in rare cases extremely stressful events, most hair loss is men can be blamed on heredity testosterone and age. What male pattern hair loss sufferers are actually inheriting are hair follicles with a genetic sensitivity to Dihydrotestosterone (DHT). Hair follicles that are sensitive to DHT begin to miniaturize, shortening the lifespan of each hair follicle affected. Eventually, these affected follicles stop producing cosmetically acceptable hair. This process of „Miniaturization” causes the terminal follicles to produce „Vellus” or baby hairs, that are fine, short and nonpigmented. Male pattern hair loss is generally characterized with the onset of a receding hairline and thinning crown. Hair in these areas including the temples and mid-anterior scalp appear to be the most sensitive to DHT. This pattern eventually progresses into more apparent baldness throughout the entire top of the scalp, leaving only a rim or “horseshoe” pattern of hair remaining in the more advanced stages of MPHL.
A CLOSER LOOK at DHT
Dihydrotestosterone (DHT) is a derivative or by-product of testosterone. Testosterone converts to DHT with the aid of the enzyme Type II 5-alpha-reductace, which is held in the hair follicle’s oil glands. While the entire genetic process of male pattern hair loss is not completely understood, scientists do know that DHT shrinks hair follicles, and that when DHT is suppressed, hair follicles continue to thrive. Hair follicles that are sensitive to DHT must be exposed to the hormone for a prolonged period of time in order for the effected follicle to complete the miniaturization process.
DIAGNOSIS
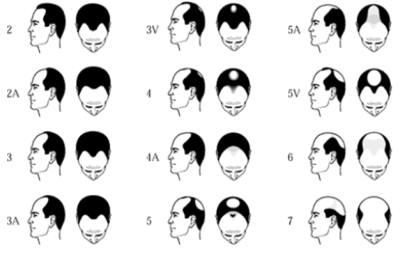
Typical male pattern hair loss is usually diagnosed based on the appearance and pattern of the hair loss along with a detailed medical history, including questions about the prevalence of hair loss in the family. At PROHAIR Transplant Clinic, an experienced doctor examines the scalp under magnification with a device called a ‘Densitometer’, in order to assess the degree of miniaturization of the hair follicles. This assessment is very important when recommending the proper course of treatment. Some advertised “clinics” might recommend a costly hair analysis or a scalp biopsy to properly diagnose your hair loss. The only reason to have a hair analysis is to assess the possibility of poison induced hair loss. A hair analysis may reveal substances such as arsenic or lead, however, hair loss caused by poising does not present itself in a typical male pattern. You should avoid these clinics and seek the advice of a doctor from PROHAIR Transplant Clinic, who can properly examine you and help you treat your hair loss. When considering treatment for your hair loss, it is important to understand just how far your hair loss has progressed. There will be times when you will have to relay this information via telephone or the internet to physicians or practitioners you may be trying to receive information from. It is also important to guard yourself against misdiagnoses of your condition.
THE NORWOOD SCALE
Note: There are many variants in pattern hair loss; these have been cited as the most typical.
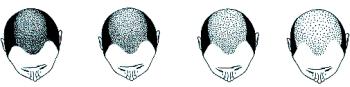
DIFFUSE PATTERNED ALOPECIA and DIFFUSE UNPATTERNED ALOPECIA
Two other types of genetic hair loss in men, as well as women, not often considered by doctors are, “Diffuse Patterned Alopecia” and “Diffuse Unpatterned Alopecia,” as they pose a significant challenge both in diagnosis and in patient management. Understanding these conditions is crucial to the evaluation of hair loss in both women and men, particularly those that are young when the diagnoses may be easily missed, as they may indicate that a patient is not a candidate for hair transplant surgery
Diffuse Patterned Alopecia (DPA) is an androgenetic alopecia manifested s diffuse thinning in the front, top and crown, with a stable permanent zone on the sides and in the back. In DPA, the entire top of the scalp gradually miniaturizes (thins) without passing through the typical Norwood stages.
Diffuse Unpatterned Alopecia (DUPA) is also androgenetic, but lacks a stable permanent zone and affects men much less often than DPA. DUPA, found more in women then men, tends to advance faster than DPA and ends up in a horseshoe pattern resembling the Norwood class VII. However, unlike the Norwood VII, the DUPA horseshoe can look almost transparent due to the low density of the back and sides. Differentiating between DPA and DUPA is very important because DPA patients often make good hair transplant candidates, whereas DUPA patients almost never do, as they eventually have extensive hair loss without a stable zone for harvesting.
The progression of male hair loss in Diffuse Patterned Alopecia (DPA) and Diffuse Unpatterned Alopecia (DUPA). In DUPA, the sides thin significantly as well.
FOR WOMEN
FOR WOMEN
INTRODUCTION
Mistakenly thought to be a strictly male disease, women actually make up forty percent of hair loss sufferers. Hair loss in women can be absolutely devastating for the sufferer’s self image and emotional well being. Unfortunately, society has forced women to suffer in silence. It is considered far more acceptable for men to go through the same hair loss process. Even more unfortunately, the medical community also treats the issue of women’s hair loss as if it were non-existent. Since hair loss doesn’t appear to be life threatening, most physicians pay little attention to women’s complaints about hair loss and essentially tell their patients that „it’s no big deal”, and that „you’ll just have to live with it”. Of course what these physicians don’t seem to realize is that the psychological damage caused by hair loss and feeling unattractive can be just as devastating as any serious disease, and in fact, can take an emotional toll that directly affects physical health.
TYPES of WOMEN HAIR LOSS
Hair loss can be temporary or long lasting. Temporary hair loss can be easy to fix when its cause is identified and dealt with or difficult when it is not immediately clear what the cause is. Hair loss that could have been merely temporary may become long lasting as a result of an incorrect diagnosis. The potential for such misdiagnoses is perhaps the most frustrating aspect of hair loss for women. The information in this section will help you identify the cause of your hair loss. Alopecia is the medical term for excessive or abnormal hair loss. There are different kinds of alopecia. What all hair loss have in common, whether it’s in women or men, that it is always a symptom of something else that’s gone wrong in your body. Your hair will remain on your head where it belongs if hormone imbalance, disease, or some other condition is not occurring. That condition may be as simple as having a gene that makes you susceptible to male or female pattern baldness or one of the forms of alopecia areata, or it may be as complex as a whole host of diseases. Fortunately, hair shedding may also be a symptom of a short-term event such as stress, pregnancy, and the taking of certain medications. In these situations, hair will grow back when the event has passed. Substances (including hormones), medications, and diseases can cause a change in the hair growth and shedding phases and in their durations. When this happens, synchronous growth and shedding occur. Once the cause is dealt with, hairs go back to their normal pattern of growth and shedding, and your hair loss problem stops.
FEMALE PATTERN BALDNESS
Dihydrotestosterone (DHT), a derivative of the male hormone testosterone, is the enemy of hair follicles on your head. Simply put, under certain conditions DHT wants those follicles dead. This simple action is at the root of many kinds of hair loss, so we’ll address it first. Androgenetic alopecia, commonly called male or female pattern baldness, was only partially understood until the last few decades. For many years, scientists thought that androgenetic alopecia was caused by the predominance of the male sex hormone, testosterone, which women also have in trace amounts under normal conditions. While testosterone is at the core of the balding process, DHT is thought to be the main culprit. Testosterone converts to DHT with the aid of the enzyme Type II 5-alpha reductase, which is held in a hair follicle’s oil glands. Scientists now believe that it’s not the amount of circulating testosterone that’s the problem but the level of DHT binding to receptors in scalp follicles. DHT shrinks hair follicles, making it impossible for healthy hair to survive.
The hormonal process of testosterone converting to DHT, which then harms hair follicles, happens in both men and women. Under normal conditions, women have a minute fraction of the level of testosterone that men have, but even a lower level can cause DHT- triggered hair loss in women. And certainly when those levels rise, DHT is even more of a problem. Those levels can rise and still be within what doctors consider “normal” on a blood test, even though they are high enough to cause a problem. The levels may not rise at all and still be a problem if you have the kind of body chemistry that is overly sensitive to even its regular levels of chemicals, including hormones. Since hormones operate in the healthiest manner when they are in a delicate balance, the androgens, as male hormones are called, do not need to be raised to trigger a problem. Their counterpart female hormones, when lowered, give an edge to these androgens, such as DHT. Such an imbalance can also cause problems, including hair loss. Hormones are cyclical. Testosterone levels in some men drop by 10 percent each decade after thirty. Women’s hormone levels decline as menopause approaches and drop sharply during menopause and beyond. The cyclic nature of both our hair and hormones is one reason hair loss can increase in the short term even when you are experiencing a long-term slowdown of hair loss (and a long-term increase in hair growth) while on a treatment that controls hair loss. The majority of women with androgenic alopecia have diffuse thinning on all areas of the scalp. Men on the other hand, rarely have diffuse thinning but instead have more distinct patterns of hair loss. Some women may have a combination of two pattern types. Androgenic alopecia in women is due to the action of androgens, male hormones that are typically present in only small amounts. Hair loss can be caused by a variety of factors tied to the actions of hormones, including, ovarian cysts, the taking of high androgen index birth control pills, pregnancy, and menopause. Just like in men the hormone DHT appears to be at least partially to blame for the miniaturization of hair follicles in women suffering with female pattern baldness. Heredity plays a major factor in the disease.
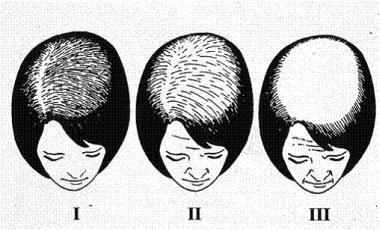
Ludwig Classification of Female Pattern Baldness